
The Basics
One in nine Texas residents is not a U.S. citizen. Census
surveys don’t record which of those 2.9 million
non-citizen residents are here lawfully, but the best
estimates are that 60 percent or more lack legal status.
Of the 5 million uninsured Texans in 2014, about 1.6
million were non-U.S. citizens. Non-citizens—even
those who are lawfully present—are not eligible for
public health insurance on the same terms as U.S.
citizens, and options for undocumented residents are
especially limited.
The 2014 roll out of the Aordable Care Act’s (ACA) new
private and public health coverage options brought
new rules and opportunities for non-US citizens. But
the law also had unintended consequences, and
barriers to care for immigrants remain signicant—
especially here in Texas. Undocumented residents are
excluded from all formal public insurance programs
(except for payment of some emergency services
in Medicaid), and legal residents face signicant
technological and legal barriers related to both public
coverage and private insurance in the new Marketplace
established by the ACA.
To reduce the confusion about which non-U.S. citizens
can access what healthcare and which programs, we
have prepared the table below. Read more about the
law, policy and history in the sections that follow.
Immigrants’ Access to Health Care in Texas:
An Updated Landscape
by Anne Dunkelberg
B
arriers to health care facing long-term resident non-citizens aect every Texan. The hospitals, clinics,
and other health care systems we all share, rely on, and nance through our taxes and insurance
premiums can only be eective if they address the health needs of all Texans, from controlling
communicable diseases to prenatal care and trauma care. Millions of U.S. citizen Texans are uninsured (the
highest uninsured number and rate in the U.S.), and our state’s large immigrant population faces all the same
barriers to care as U.S. citizens, plus an additional complex list of exclusions. The eects reach far beyond any
individual immigrant. One-third of Texas children have a foreign-born parent, and foreign-born workers and
small employers in Texas make hefty contributions to our state economy (see: Immigrants Drive the Texas
Economy: Economic Benets of Immigrants to Texas). When individual immigrants are disenfranchised from
access to health care it can aect whole families, and the health and prosperity of the communities in which
they live, work, study and worship. Like any other uninsured Texan, immigrants who delay getting care too
often end up needing costly emergency care on the local taxpayer’s tab.
October 2016
In This Report
• Texas Choices: Immigrants and Public
Health Care Programs
• Non-Citizens in Texas: A look at the
Numbers
• Helpful Immigration Terms
• Table: Immigrants’ Access to Health Care
in Texas, 2014
• Why Fears of Immigration Consequences
Cause Some to Avoid Health Care
• ACA Extends Aordable Marketplace
Coverage to Lawfully Present
• Undocumented Residents: Federal and
Texas Policy
• Rights and Rules When Mixed-
Immigration Families Apply for Health
Care
• ACA Marketplace: Coverage and
Challenges for Mixed-Immigration
Families
• Recap: Focus on Gaps in Access to Care
for Immigrants in Texas
• APPENDIX: Immigrants and Health Care:
Federal Policy Basics
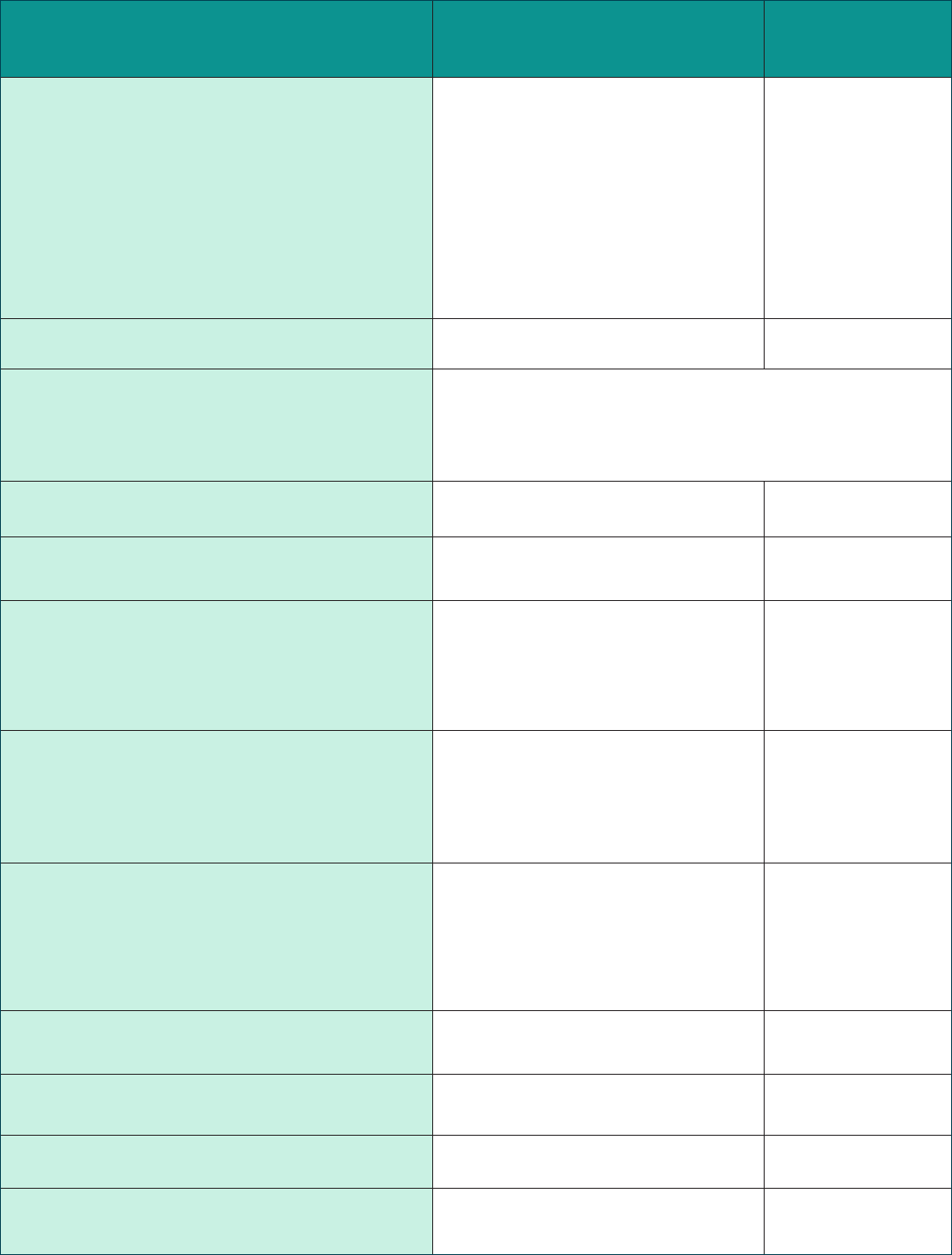
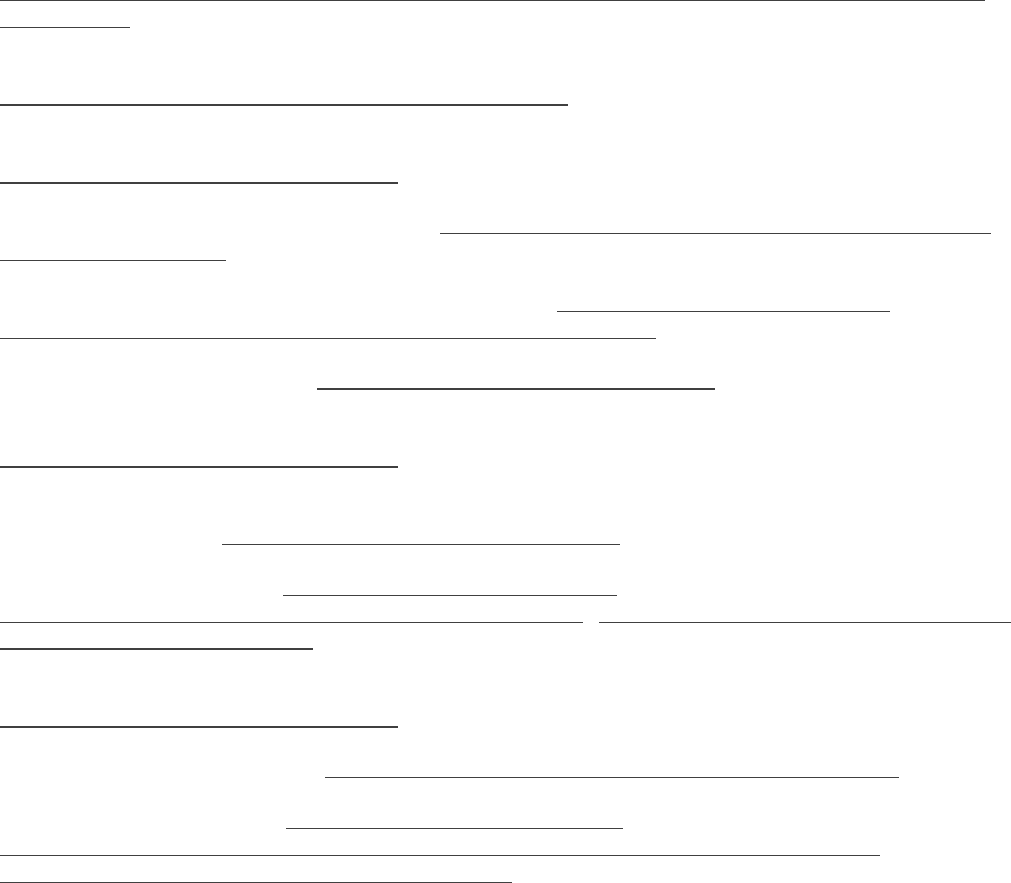
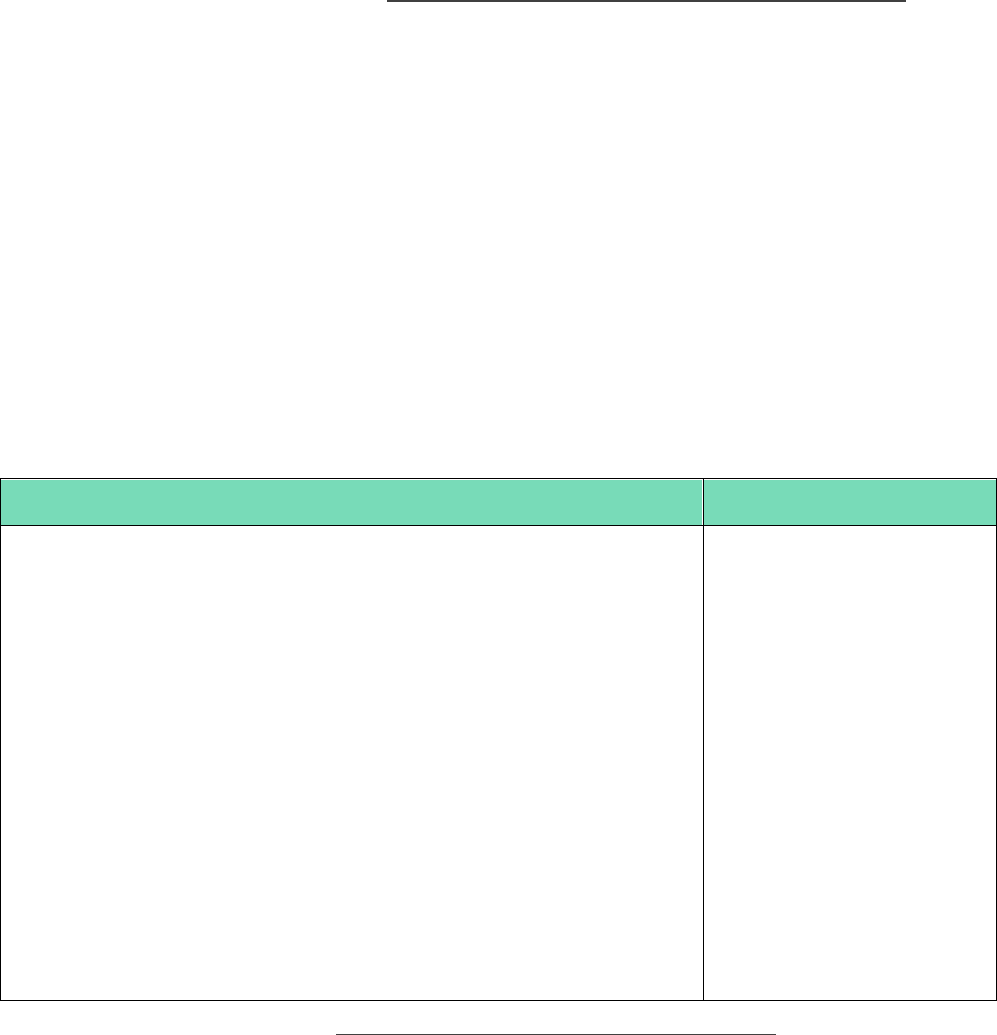
Table 1: Immigrants’ Access to Health Care in Texas, 2016
Health Care Program or Service
Lawfully Present
Immigrants
Undocumented
Immigrants
Medicaid-Adults 19 and older
NO for most immigrants who came
to U.S. on or after 8/22/1996
YES, for immigrants before
8/22/1996, but limited to same
categories as U.S. citizens (very few
parents qualify, and no adults without
dependent children unless pregnant,
senior, or disabled)
NO
Medicaid-Children under age 19 YES NO
“Emergency Medicaid”- pays care providers
for emergency care only (not full coverage)
YES, but only ER bills for individuals who, except for immigration status,
meet all the same strict TX Medicaid limits that apply to U.S. citizen
adults (very few parents qualify, and no adults without dependent children
unless pregnant, senior, or disabled)
CHIP-Children under age 19 YES NO
CHIP Perinatal Program-prenatal, delivery,
and postpartum care
YES YES
Refugee Medical Assistance
Medical assistance to refugees for up to 8 months from
the individual’s legal date of entry (those who apply
after their legal date of entry month receive less than 8
months of RMA coverage).
YES
Must have a U.S. CIS
veried refugee status
NO
Programs using federal health care block
grant funds (includes those run by state, county or
city): Examples: mental health, maternal and child health,
family planning, communicable diseases, immunization
YES YES
Programs providing health services
necessary to protect life or safety, includes
those using federal, state or local funds. Emergency
medical, food, or shelter, mental health crisis, domestic
violence, crime victim assistance, disaster relief
YES YES
County Hospital or Health Districts and
Indigent Care Programs
YES VARIES by County
Marketplace Insurance Coverage, with
subsidies
YES NO
Marketplace Insurance Coverage, no subsidy YES NO
Insurance purchase outside Marketplace,
no subsidy
YES YES

W
ith over 4.6 million uninsured Texans in
2015, substantial gaps in access to health
care will remain a problem for many Texans
in the near term, despite the important gains and
new options provided by the ACA. Listed below is a
partial inventory of notable holes in the Texas health
care safety net for non-U.S. citizen residents.
Undocumented. The greatest access gaps for non-
citizens aect Texans without legal immigration
status. Barred from Medicaid, CHIP, and the
Marketplace and its subsidies, private health
coverage is available only to undocumented
individuals who have adequate income to
purchase a policy at full price, without a subsidy.
Undocumented residents can look to Federally
Qualied Health Centers, some (but not all) urban
hospital/health districts, and independent charity
clinics for care, meaning that access to aordable
care is highly variable depending on where an
immigrant lives in Texas.
Lawfully present: Immigrants who are lawfully
present in the U.S. face certain barriers that are
specic to their non-citizen status, as well as some of
the same barriers aecting U.S. citizens.
● The Coverage Gap traps some lawfully present,
including refugees and asylum seekers. Most
lawfully present individuals with incomes below
100 percent of the FPL can qualify for subsidies in
the ACA Marketplace. However, certain lawfully
present immigrants are caught in the Coverage
Gap in states like Texas that have not accepted
federal ACA funds to extend Medicaid to adults
who earn less than 138 percent of the FPL. So
the categories of legal immigrants that Congress
intended in 1996 to have access to Medicaid
and CHIP, actually are the very ones who are left
without coverage options in Texas and other
states that have not expanded Medicaid.
● Texas law excludes most lawfully present
immigrant adults from Medicaid. The state
legislature would have to authorize a change to
this state policy (adopted in 1999) in order for a
Texas solution to insure low-income Texans in
the Coverage Gap to also benet lawfully present
adults below the poverty line.
● Technical Marketplace application processing
issues for individuals with immigration
documents, as well as for mixed-status families
have delayed coverage and discouraged eligible
Texans from completing enrollment. Improved
Marketplace performance during the second
and third open enrollment period appears
to be improving enrollment rates but further
improvement is still needed.
● The “family glitch” aects both lawfully present
immigrants and U.S. citizens. These families
may not qualify for premium subsidies in the
Marketplace , and face either paying full price and
an unlimited, unaordable percentage of their
incomes for job-based or Marketplace insurance
premiums, or remaining uninsured.
● Aordability issues occur even for families that
have access to premium subsidies and out-of-
pocket help in the Marketplace. Those below
poverty may have a hard time aording 2
percent of income in premiums with additional
copayments and deductibles. Families at any
income level who experience high health care
needs may face spending up to 20 percent of
income before deductibles and out-of-pocket
caps kick in.
● Separated, but not divorced, parents may not
have access to Marketplace subsidies because
of tax ling status or lack of access to income
information on the absent spouse.
● Hard-to-verify incomes. The income verication
systems that the Marketplace and state Medicaid-
CHIP programs rely on can work well for those
with steady employment and predictable hours
and wages. They are less helpful for those working
irregular hours, multiple jobs, or being paid cash
or by hand-written check. Advocates will need to
monitor the systems to identify and try to reduce
any barriers to enrollment, renewal, or qualifying
for premium subsidies that may result from
the additional documentation families in these
situations may have to produce on an ongoing
basis.
Executive Summary
Key Findings and Recommendations for Texas

How to use this report to protect access to care in your community
Why This Report?
This report provides an updated overview of federal and state laws and rules governing access to health care in Texas
for non-U.S. citizens, and points out how local practices vary around the state. With a new presidential administration
beginning in January 2017, changes to weaken protections in federal laws and rules could be proposed in the near future.
Attempts to make health care less accessible to non-U.S. citizens are on the rise. In the past, health care stakeholders in
Texas avoided direct talk about the programs and services available to non-citizens—even those lawfully present—in
hopes that silence would reduce attacks on immigrants’ health care access. At CPPP, we believe that given the increased
frequency of attacks on access, silence is no longer serving that end. Health care providers, community advocates,
congregations, and concerned citizens all need to be armed with the facts about federal, state, and local laws and the
rights of immigrants. Only armed with this information can we ensure that laws are followed and rights are protected.
CPPP is available to help educate organizations and community members, and to hear reports from those who observe
violations of law or policy, or need help understanding if a violation has occurred. Information on how to contact us is at the
end of this report.
Recommendations to Improve Health Care
Access and Outcomes
Federal law, Texas law and the state constitution combine
to make Texas cities, counties, and hospitals the providers
and funders of last resort for all of the uninsured. U.S.
and Texas law allow federal and state government to
reject the health costs of uninsured immigrants—lawfully
present and undocumented alike—and shift them to
local governments and health care providers. In this way,
Texas’ policy decisions to turn down available federal
support for the uninsured take a toll on local taxpayers,
and on all the other services communities need to fund.
CPPP recommends that Texas make the following three
key policy changes to increase federal funding for
coverage and care of immigrants:
1. Providing Medicaid Maternity benets to lawfully
present immigrant women. Texas should provide
comprehensive pregnancy benets on par with those
of U.S. citizens. Today, even legal permanent residents
are treated the same as undocumented mothers.
2. Closing the Texas Coverage Gap, and insuring all
citizens 19-64 up to 138 percent of the federal
poverty line ($27,724 for a family of 3). This step
would do even more than #1 for maternal health, by
allowing women access to medical homes before
conception for healthier pregnancies, continuing their
care after birth to screen for and treat chronic medical
conditions, and thereby improving health for any
future pregnancies. This improved care will be gained
equally if accomplished via an 1115 “red state waiver”
conservative alternative.
Closing the Gap will also eliminate today’s perverse
policy which denies access to coverage to immigrants
Congress intended to protect: e.g., active-duty
military and veterans, victims of human tracking,
and refugees. Step #2 will also dramatically improve
payments to hospitals and doctors for emergency care
to uninsured undocumented residents.
3. Providing Medicaid benets to lawfully present
immigrants aged 19 and older. Lawmakers should
also reverse the Texas law that now excludes these
adults, in order to maximize the reduction in uninsured
lawfully present Texans and the relief for local
governments that closing the Coverage Gap would
bring. Texas Medicaid today covers very few U.S. citizen
parents and adults under current policy: e.g., 3 million
children are enrolled, but only 150,000 of their parents.
Unless Texas begins providing coverage options for
U.S. citizen parents and other adults living in poverty,
reversing Texas’ ban on Medicaid for lawfully present
immigrant adults will have limited eect.
Of course, the steps described above do not fully address
the barriers to care for undocumented residents and the
costs of their care born by local governments and care
providers. Texas should take the lead among the states,
squarely face the realities and negative consequences
of these barriers for our communities, and develop a
proactive strategy to improve systems and nancing of
care for the undocumented uninsured.
CENTER FOR PUBLIC POLICY PRIORITIES • CPPP.org • 5123200222
CPPP_TX
BetterTexasBlog.org BetterTexas
Immigrants’ Access to Health Care in Texas: An Updated Landscape
5
Texas’ Choices: Legal Immigrants and Public Health Care Programs
See Appendix and Resources for more detailed federal policy background.
1997: Texas Denies Medicaid to Most Recent Legal Immigrants.
The Texas Legislature opted in 1997 to continue providing Medicaid to “qualified immigrants” (see Helpful
Immigration Terms box, p. 3, and Appendix) who came to the U.S. before the 1996 federal welfare law known as
the Personal Responsibility and Work Opportunity Reform Act (PRWORA, 8/22/1996). But the state Legislature
decided to exclude qualified immigrants who came to the U.S. after that date, even when they have been in the
U.S. for five years and qualify for federal Medicaid funding. (In 2001, the Legislature passed an omnibus
Medicaid bill that would have reversed that decision and allowed post-1996 qualified immigrants to qualify for
Texas Medicaid, but that bill was vetoed by the Governor).
Non-Citizens in Texas: A Look at the Numbers
THE BIG PICTURE: U.S. Census estimates non-U.S. citizens made up 2.9 million of the 26.9 million Texans in 2014
(Census, American Community Survey).
U.S. Census does not determine which non-citizens are lawfully present and which are not.
68% of foreign-born Texans (including naturalized U.S. citizens) are of Latin American origin, 18% Asian. (Migration
Policy Institute (MPI), 2014.)
UNDOCUMENTED: Pew Hispanic Center estimates Texas was home to 1.7 million undocumented immigrants in 2012;
MPI estimates about 1.5 million for 2014.
The U.S. unauthorized immigrant population peaked in 2007 at about 12.2 million.
Since 2008 the national total has declined by about 1 million and more undocumented immigrants have left the
state than have moved here, due to the global recession, increased border security, and greater risk to migrants
from criminals.
The drop was due mostly to reduced immigration from Mexico.
Additional sources: Pew Hispanic Center, Statistical Portrait of the Foreign-Born Population in the United States,
September 2015; 5 facts about illegal immigration in the U.S., November 2015.
CHILDREN:
Though only 4% of Texas children are themselves foreign-born, in 2014 2.4 million Texas children (one-third of Texas
children) had a foreign-born parent (Annie E Casey Foundation Kids Count project estimates).
o Half of these children are in families in which neither parent is a U.S. citizen (includes both lawfully present
and undocumented parents).
o Of Texas children in these mixed-status families, 33% live below the poverty line ($20,160 for a family of 3),
compared with 25% of all children.
The Migration Policy Institute estimates that 45% of all low-income Texas children (those with family income below
200% FPL, which is the upper limit for the Children's Health Insurance Program (CHIP), $40,320 for a family of 3)
have at least one foreign-born parent.
The Texas Medicaid program reports it covered costs for 213,253 Texas births in 2013.
o That year, Texas Medicaid paid for deliveries for about 159,000 U.S. citizen mothers.
o About 26% of Texas Medicaid births in 2013 were to non-U.S citizen mothers (about 55,000, includes both
lawfully present and undocumented mothers), representing about 15% of all Texas births that year.
6
1999: Texas includes Legal Immigrant Children in CHIP
The option for each state to create a Children’s Health Insurance Program (CHIP) was established by Congress in
1997 when the Texas Legislature was not in session, and the Legislature enacted CHIP coverage in 1999 in its next
regular session. The federal law required Texas to include qualified immigrant children who have been in the U.S.
for at least five years in our separate (non-Medicaid) CHIP program, but provided no federal funding for those
children during their first five years in this country. The Texas Legislature opted to use 100 percent state funds to
cover qualified immigrant children in CHIP during their first five years in the U.S. when no federal match was
available, convinced that promoting early intervention and a regular source of medical and dental care for
children would be cost-effective in the long run.
Helpful Immigration Terms
“Alien” is a term used in many laws to refer to noncitizens (both lawfully present and undocumented).
“Undocumented” Immigrants include 2 major groups, people who:
Entered Without Inspection, or “EWIs”
Overstayed their immigrant or nonimmigrant visas; these make up 25-40 percent of all undocumented immigrants
Other terms you may see: “not lawfully present,” “illegal aliens” (the latter term is not preferred or used in this report)
“Legal Immigrant” – not a real term in law, but still is commonly used. There are many different lawful immigration
statuses:
Some are permanent or long-term statuses; that is, the immigrant can reside in the U.S. indefinitely. Includes
Lawful permanent residents (LPRs), refugees, and asylum seekers (“asylees”).
Others are temporary, or transitional statuses, which may be indefinite in length (for example, the spouse, child
or fiancée of a U.S. citizen waiting to get LPR status may have a “K” Visa), or they may be required to get approval
for renewal of status at regular intervals (e.g., “Temporary Protected Status”).
Most LPRs immigrated through a family-based immigrant visa petition.
All lawfully present immigrants are not treated equally with regard to access to health care.
NOTE: “qualified” and “lawfully present” immigrants have different specific meanings in law and policy. They are
italicized in this report when they refer to a specific legal or regulatory definition.
“Qualified” Immigrants
A specific group of immigration statuses that was designated in the 1996 federal welfare law for the purpose of
establishing new restrictions on eligibility for public benefits. (See appendix for detail)
“Lawfully Present” immigrants
Federal categorization of immigrants who are potentially eligible for Medicaid and CHIP under the state option to
cover children and pregnant women established in 2009 federal law (under the Children's Health Insurance
Program Reauthorization Act, CHIPRA), and for Marketplace insurance under the Affordable Care Act. It includes
almost all legal statuses, including non-immigrants with valid visas. (See appendix for detail)
The words “lawfully present” are sometimes also used to refer generically to non-U.S. citizens who are not
unauthorized. In this report we italicize lawfully present when it is used to refer to the specific grouping of lawful
statuses established in federal law and policy related to access to health care and insurance programs.
“Immigrant” versus “Nonimmigrant” visas
“Immigrant” statuses include people seeking long-term or permanent residence.
Tourists, students, people conducting business, temporary employees, or those traveling to the U.S. to receive
medical care are the primary examples of “non-immigrant” status.

7
By 1999, federal legislation had already been introduced in response to PRWORA to give states the option to
eliminate the five-year bar from Medicaid and CHIP for immigrant children and pregnant women. The authors of
Texas’ CHIP law therefore included a “trigger” in Texas law directing the program to accept federal funding for
immigrant children in their first five years, should Congress ever adopt that bill and make that option available.
Today: Where Medicaid and CHIP stand in Texas
Qualified immigrants who entered the U.S. before August 22, 1996 may participate in Medicaid on the
same terms as U.S. citizens.
Most qualified immigrants ages 19 and older who entered the U.S. on or after August 22, 1996 are not able
to access Texas Medicaid (see Appendix for exceptions).
o Texas is one of just six states that exclude qualified immigrant adults from Medicaid if they came to
the U.S. after the 1996 federal welfare law took effect. (Alabama, Mississippi, North Dakota, Virginia,
and Wyoming are the others).
o This Texas policy means Medicaid maternity coverage is not available to qualified immigrant women.
Instead, these women are treated the same as undocumented immigrant women. They can
participate in the “CHIP Perinatal” program, which provides prenatal visits and limited postpartum
care, and “Emergency Medicaid” (more below) will pay the bill for labor and delivery. They cannot get
coverage with more comprehensive pre-conception care or postpartum health care.
Texas also has extremely limited Medicaid coverage for adult U.S. citizens, because the state has not yet
accepted the federal funds available under the ACA to cover most U.S. citizen adults with incomes below 138
percent of the federal poverty income level ($27,821 for a family of 3). But even with the current limits in
place for U.S. citizen adults, tens of thousands of pregnant women and thousands of parents could gain
comprehensive health benefits if Texas stopped excluding qualified immigrant adults who came here on or
after August 22, 1996 from Medicaid coverage.
If the state moves forward to accept the coverage of all U.S. citizen adults up to 138 percent FPL, taking the
additional step of ending the exclusion of adult qualified immigrants from Texas Medicaid would be needed,
to provide affordable coverage to legal immigrant adults in that income group.
Lawfully present immigrants 18 and younger may participate in Texas Children’s Medicaid and CHIP on the
same terms as U.S. citizen children. When Texas CHIP was launched in 2000, all qualified immigrant children
with incomes below 200 percent of the federal poverty income were enrolled in CHIP (not Medicaid). When
Congress passed the Children's Health Insurance Program Reauthorization Act in 2009 (CHIPRA), it created the
option for states to get federal matching funds for children and pregnant women without a 5-year wait. As
directed by Texas’ 1999 CHIP law, Texas Medicaid and CHIP then implemented the option to accept the
federal funds for children in Medicaid and CHIP (but not for pregnant women), without a 5-year wait.
Congressional CHIP Reauthorization in 2009 also extended the categories of eligible immigrant children to the
broader group of lawfully present children (see Appendix). Lawfully present immigrant children today are
covered in Texas Medicaid and CHIP according to the same income guidelines as U.S. citizen children.
8
Importantly, under the CHIP Reauthorization, the U.S. “sponsors” of immigrant children and pregnant women
covered in Medicaid or CHIP are not liable for repayment of health care costs, and a sponsor’s income is not
counted as part of the immigrant’s income for eligibility purposes (see below, Sponsor Income and Liability,
and Fears of Immigration Consequences).
CHIP Perinatal Program. Texas authorized the CHIP Perinatal program in 2005 using CHIP funding to provide
prenatal visits and limited postpartum care to both lawfully present and undocumented immigrant mothers
with incomes below 200 percent of the federal poverty line ($40,320 for a family of three), because they are
excluded from Medicaid Maternity coverage. Emergency Medicaid (more below) pays the bill for labor and
delivery. (CHIP perinatal also is available to U.S. citizen mothers with incomes between 185-200 percent of the
FPL).
State and Local Health Care Programs. Federal law and regulations provide access to all other health care
programs—such as maternity care, mental health, immunizations, disease control—for qualified immigrants
(see Appendix). Importantly, state and local health programs cannot add their own immigrant restrictions to
any public health programs that use those unrestricted federal funds. Texas operates relatively few public
health programs that do not mix federal funds with state dollars.
The most common locally funded and operated health care programs in Texas are hospital and health district-
funded medical assistance programs typically found in the largest urban counties, and the County Indigent
Health Care programs in most smaller-population counties without hospital or health districts. Texas Hospital
Districts do have an obligation under both state law and the Texas Constitution to serve all needy residents.
As a general rule, local health care programs have not restricted access by qualified immigrants.
Individuals with “non-immigrant” status (such as student, tourist, and employment visa holders) are required
to prove that they are residents in some Texas localities in order to use these health care programs. What is
accepted to prove residency differs from place to place, but in some locales includes rent receipts or utility
bills, to establish some intent to reside in the community. Federal rules for Medicaid and the Health insurance
Marketplace prohibit state Medicaid programs or Marketplaces from defining a person to be a non-resident
based strictly on their immigration status or type of visa.
i
The federal rules represent a fairly new best
practice, and may influence Texas counties to update their policies in places that reportedly still assign non-
resident status to immigrants based solely on their visa type.
Sponsors’ Income and Liability. Many Lawful Permanent Residents (often called “green card” holders) are
sponsored by a relative or others who promise to help provide for the new immigrant’s needs. In 2011, the
state Legislature adopted a new law allowing county health care programs to count (“deem”) the income and
resources of immigrants’ sponsors when determining if an immigrant is eligible for a Hospital District or
County Indigent Health Care program. The same legislation also gave those programs the option to recover
costs of care from the sponsors, and directed the Texas Medicaid program to do the same if cost effective. Of
course, counting the income of a separate household as though it were available to the immigrant reduces
the ability of an immigrant family to qualify for care. It’s not known how common the practice is in Texas,
since at this time it appears that no state entity maintains a centralized record of the policies adopted by local
governments.
9
ACA Extends Affordable Marketplace Coverage to those Lawfully Present
When the ACA was passed in 2010, it made the same group of “lawfully present” immigrants defined in the 2009
CHIP Reauthorization eligible to participate in the new health insurance Marketplace in 2014. Those with incomes
below four times the federal poverty line income ($80,640 for a family of three in 2016) can qualify for reduced-
cost insurance through lower premiums (subsidized with “premium tax credits”) and reduced out-of-pocket costs
(“cost-sharing reductions”) for families with incomes below 250 percent of the federal poverty line. Just like U.S.
citizens, lawfully present immigrants who are offered “affordable” job-based coverage do not have access to
marketplace subsidies (more later, see “Family Glitch”).
Why Fears of Immigration Consequences Cause Some to Avoid Health Care
Fear of being Labeled a “Public Charge”
Some immigrants fear that using publicly sponsored health care or subsidies will prevent them from getting legal
status or citizenship. Federal policy in place since 1999 has tried to reassure non-citizens that use of health care by
eligible people will not create barriers to immigration or citizenship, but confusion and fear remain among both
undocumented and lawfully present immigrants.
The only way health care use can prevent a green card holder from becoming a citizen is if he or she committed
fraud to get those benefits (for example, misrepresented his or her income, state residence or immigration status).
Sponsor “deeming” and liability
Many Lawful Permanent Residents (sometimes called “green card” holders) are sponsored by a relative or others who
promise to provide for the new immigrant’s needs. In some situations, the sponsor’s income can be counted
(“deemed”) as if available to the sponsored person in determining eligibility for health care services. And though
asking sponsors to repay the costs of care (“liability”) provided to those they sponsor is almost unheard of, it is
technically possible under the law in some cases and thus creates a barrier for some immigrants. Care for children in
Texas CHIP or Medicaid is exempt from sponsor deeming and liability.
Reporting to the U.S. Citizenship & Immigration Services (USCIS, formerly INS)
Medicaid, CHIP, other health programs and health care providers are not required to report all undocumented
persons to immigration authorities. Indeed the Department of Homeland Security has confirmed that it will not use
information provided by health care applicants for immigration enforcement purposes. Reporting to USCIS can occur
in cases of fraud, but is not done simply based on a household including a person with undocumented status. Still,
immigration officials have on occasions been known to seek out immigrants in health care settings, which can create
long-lasting fears spread by word of mouth, and make immigrants reluctant to get necessary care.
Congress intended for all U.S. citizens aged 19 to 64 and with incomes up to 138 percent FPL to qualify for
Medicaid in every state. The ACA’s Marketplace subsidy provisions limited premium assistance to U.S. citizens at
or above the poverty line (100 percent FPL), on the assumption that all U.S. citizens below that income would
qualify for Medicaid. But after the U.S. Supreme Court removed any penalty for states failing to implement the
expanded Medicaid for adults, a number of states have left their uninsured U.S. citizen adults below poverty who
don’t qualify for Medicaid without an affordable option. As of March 2016, 19 states (including Texas) had not yet
taken action to cover the poorest uninsured in this “Coverage Gap,” though several of those states have active
debate underway on the topic. The Supreme Court decision only eliminated fiscal penalties for states that did not
expand Medicaid coverage to 138 percent of FPL, but made no other changes to the ACA. Thus, the law still only
allows subsidies to U.S. citizens above the poverty line, even in states with no Medicaid coverage assistance for
adults in families with poverty-level incomes.
10
Most Lawfully Present Immigrants Escape the Coverage Gap
Congress intended for lawfully present immigrants, including qualified immigrants in the “5-year bar,” to have
access to affordable healthcare, so the ACA allowed these lawfully present immigrants below the poverty line (100
percent FPL, $20,090 for a family of three) to qualify for subsidies in the Marketplace. Under the ACA, a lawfully
present immigrant below poverty can qualify for Marketplace subsidies if they were excluded from Medicaid
because of immigration status.
Texas excludes most qualified and lawfully present immigrant adults (age 19 and older) from Medicaid (exceptions
include pre-1996 immigrants and several categories of federally mandated exceptions). Because of this exclusion
on the basis of immigration status, most qualified immigrant adults in Texas with incomes below 400 percent
FPL—including those with incomes under the poverty line—can qualify for financial help in the ACA Marketplace.
Access to Marketplace coverage, including premium tax credits and cost-sharing reductions, is not subject to a
five-year waiting period.
The unintended result of the Supreme Court’s ruling on Medicaid is that in non-expansion
states, most lawfully present immigrants with incomes below the poverty line can gain
access to the Marketplace premium and cost-sharing subsidies, while their U.S. citizen
neighbors with the same income cannot. In fact, when Arizona’s Governor adopted Medicaid
Expansion, she cited the desire to eliminate this inequity as one of her reasons.
….But Some Lawfully Present do Fall Into Coverage Gap
The ACA’s exception that allows lawfully present immigrants below 100 percent FPL access to subsidies (that is,
even though U.S. citizens at that income are denied) applies in cases where the immigrant is denied Medicaid on
the basis of immigration status. As described in the appendix, access to Medicaid for certain qualified
immigrants—e.g., active military, refugees and people granted asylum during their first 7 years in the U.S., and
survivors of human trafficking—was protected in 1996 law, so they are treated like U.S. citizens for purposes of
Medicaid eligibility.
Ironically, because these individuals are not excluded from Texas Medicaid based on their immigration status, but
instead are only excluded because of Texas’ failure to date to establish Medicaid coverage for adults, they fall into
the Coverage Gap along with their U.S. citizen peers.
So the categories of legal immigrants that Congress intended in 1996 to have access to
Medicaid and CHIP, actually are the very ones who are left without coverage options in
Texas and other states that have not expanded Medicaid.
Rights and Rules When Mixed-Status Families Apply for Health Care
• Only the individual applicant's immigration status is relevant to his eligibility; for example, a parent's
immigration status does not affect a U.S. citizen child's eligibility for public benefits.
• Medicaid, CHIP, and the Marketplace do not, and may not, require either a Social Security Number or
immigration status information from parents who are applying for health care for their children, and not
for themselves—or from any other non-applicant household members.
• Medicaid, CHIP and the Marketplace will ask parents who do have a valid Social Security Number to
voluntarily provide it. Individuals should provide only valid Social Security numbers that were issued to
them by the Social Security Administration.
• A U.S. citizen or lawfully present person who is applying for coverage for themselves can be required to
have—or to apply for—a Social Security Number to get Medicaid or CHIP.

11
Undocumented Residents
Undocumented Residents and Health Care Access: Federal Policy Basics
Undocumented residents have never qualified for Medicare, Medicaid, or CHIP enrollment with full benefits.
However, Medicaid does include an important program that pays emergency medical bills of some immigrants
who are excluded from full coverage. Most other non-entitlement federally funded health care programs—like
immunization, mental health, prenatal care, and community health centers—are by law open to all who qualify
based on need, and without restrictions based on immigration status. Federal CHIP regulations allow states to
fund prenatal care for immigrant mothers excluded from Medicaid themselves, but whose children when born will
be CHIP- or Medicaid-eligible as U.S. citizens.
Emergency Medicaid. The slightly misleading name of this program results in some common misunderstandings
about what it does, and for whom. Federal law requires that all state Medicaid programs pay Medicaid care
providers for emergency medical care they provide to people who meet all the state’s eligibility requirements
except for citizenship or immigration status.
Key facts often misunderstood include:
Only bills for patients who meet all of Medicaid’s same income and other requirements that would apply
to a U.S. citizen (that is, people who qualify in every other way but for immigration status) can be paid, so
many emergency care bills for undocumented immigrants do not qualify for coverage.
Covered services typically are limited to services provided in the Emergency Department for medical
emergencies, with the important addition that covered emergency care services are specifically defined in
federal law to include labor and delivery.
As a general rule, states do not enroll undocumented residents or issue Medicaid cards for Emergency
Medicaid. Instead, patients apply through their health care providers for their emergency care bills to be
paid.
Emergency care for lawfully present immigrants is also reimbursed by this program in Texas, and the
other five states that exclude legal immigrants from Medicaid eligibility.
Despite its broad-sounding name, the Emergency Medicaid program does not cover any emergency
medical bills for uninsured U.S. citizens; it is only for those bills of non-citizens excluded from Medicaid.
Other Federal Health Care Block Grants are Generally Not Restricted. The 1996 welfare and immigration laws
established new guidelines for undocumented residents’ access to federally funded health care from other
programs. A special set of guidelines applies to the non-entitlement federal health and human services programs,
mostly federal block grants and other public health and mental health spending.
Two major provisions shape the continued availability of public health services for undocumented residents. One
PRWORA provision declared that “not qualified immigrants” would be denied “federal public benefits.” Here, “not
qualified” meant all of the non-citizen statuses not included in the “qualified immigrant” list (see Helpful
Immigration Terms box and Appendix). However, most federal block grant programs that are focused primarily
on health care are not classified as federal public benefits, and so are not subject to immigration-status-based
restrictions. For example, federal maternal and child health, family planning, mental health and substance abuse,
and community health center funding were not subject to the new requirement. Federally-funded programs
providing these services do not, and in fact may not, exclude the undocumented. State and local programs that
supplement these federal funds with local revenues may not add their own immigration-related exclusions.

12
Essential Services that May Not Exclude Undocumented. A second key PRWORA provision directs that public
programs, whether federal, state or local, must not restrict access based on immigration status if they provide
any of the following:
Emergency Medicaid; and immunizations, or diagnosis (including testing) and treatment of communicable
disease (outside of Medicaid);
Shelters, soup kitchens, crisis intervention, and other non-cash assistance that is needed to protect life
and safety and is not limited to those with low incomes; or
Short-term, non-cash emergency disaster relief.
Public programs (and service providers) performing these functions not only are not required to verify
citizenship or immigration status (with the exception of Emergency Medicaid), they actually may not exclude
people because of immigration status.
Official federal standards explicitly name “medical and public health services, and mental health, disability or
substance abuse services necessary to protect life or safety” as services that must be available to all in need.
Federal guidance has clarified that even where a block grant is classified as a “federal public benefit,” some of the
services provided by the grant may be exempted, and therefore not restricted based on immigration status. This
protection “trumps” any exclusion of undocumented persons from a “federal public benefit,” so that for example
Title XX funding for a domestic violence shelter may be used for all victims regardless of immigration status, even
though Title XX is a “federal public benefit.”
Federally Qualified Health Centers are a critical source of care for low- and moderate-income mixed-status
families, because they combine comprehensive primary care resources with sliding-scale fees, accept Medicaid
and CHIP, and do not exclude non-citizens. They receive only limited federal funding for care for the uninsured,
so Texas’ decisions to limit Medicaid coverage of adults—both for U.S. citizens and for lawfully present
immigrants—increase the demand for those limited funds for the uninsured, putting pressure on the centers’
fiscal viability and their capacity to serve the remaining uninsured.
ACA Excludes Undocumented Immigrants from Marketplace Purchasing and Subsidies. Under the ACA,
individual undocumented residents may not enroll in coverage through the new state and federal Marketplaces,
and they do not qualify for premium or cost-sharing subsidies (these exclusions do not affect family members of
an undocumented person who are U.S. citizens or lawfully present non-citizens). Because they are excluded from
Medicaid, CHIP and the Marketplace, undocumented residents are also exempted from tax penalties for the
uninsured.
Key Federal Rules Insuring Access to Communicable Disease and Emergency Care
Together, the two provisions mean:
• All federal, state, and local programs—regardless of the funding source—that provide emergency or
crisis care, diagnosis or treatment of communicable disease, or immunization are open to non-U.S.
citizens regardless of their immigration status; and
• Any health program using federal health care funds—except for Medicaid and CHIP—must serve both
lawfully present and undocumented residents.

13
Texas Policy and Practice: Health Care Access for Undocumented Residents
Because of Texas’ high number of residents without health insurance (4.6 million uninsured in 2015, 17.1 percent
of Texans of all ages), local governments play a big role in connecting some of the neediest uninsured with health
care. However, though they generally meet the minimum federal and state legal standards regarding inclusion of
immigrants, local health care safety net programs in Texas vary considerably in whom they serve and what
services they provide.
Access to Emergency and Communicable Disease Care is Assured. As described above, federal law and guidance
forbid state or local programs from denying certain types of care “necessary to protect life or safety” based on a
person’s immigration status. And, state and local programs that co-mingle state or local revenues with federal
health care block grant funding may not deny care to undocumented immigrants in those programs. However,
federal law does permit state and local programs to exclude the undocumented in some circumstances, including
when the services provided are not necessary to diagnose or treat communicable disease or to protect life and
safety, and when no federal funds are used for the program.
Local Texas County Indigent and Hospital District Programs Choose Whether to Provide Comprehensive Care.
Policies of Texas Hospital Districts and County Indigent Health Care Programs to limit care for the undocumented,
and local practices regarding optional sponsor deeming and liability for qualified immigrants vary widely across
the state. A recent informal query of urban hospital district policies found that most of Texas’ largest urban
districts include undocumented residents in their programs for the uninsured, while most districts in the smaller-
population urban counties do not.
To comply with federal law, any counties that choose to exclude the undocumented from
their programs for the uninsured must nevertheless provide access to emergency care,
immunizations, diagnosis and treatment of communicable disease, and any other health
care interventions needed to protect life and safety, to all residents regardless of
immigration status. This requirement applies regardless of whether federal funds are used
by the county program.
Texas CHIP Perinatal Program: Prenatal, Delivery, and Postpartum Care. Federal law excludes all undocumented
residents from Medicaid, except via the Emergency Medicaid provisions. And, as explained above, Texas Medicaid
also excludes lawfully present pregnant women from full Medicaid maternity benefits. Federal and state funding
for prenatal care for women (e.g., Maternal and Child Health Block Grant, Title V) who are ineligible for Medicaid
historically was not adequate to meet Texas’ statewide need.
When a new CHIP option was created by federal regulation to provide prenatal care to the mother, on behalf of
the unborn future CHIP- or Medicaid-eligible U. S. citizen child, Texas adopted it. Approved by the state
Legislature in 2005 and launched in 2007, this program provides prenatal care benefits to both undocumented
and lawfully present immigrant mothers excluded from Texas Medicaid (as well as uninsured U.S. citizen women
between 185 and 200 percent of the FPL whose incomes are just above the upper limits for Medicaid maternity
benefits). Texas’ CHIP Perinatal program provides prenatal visits and limited postpartum care, with Emergency
Medicaid paying the bill for labor and delivery when the mother is a non-US citizen.
Birth Certificates for U.S. Citizen Children with Undocumented Parents. Birth certificates are issued in Texas by
local registrars, under authority and supervision of the Texas Department of State Health Services (DSHS). Several
years ago, changes in state rules and policies resulted in the rejection by local registrars of many of the identity
documents accessible to the undocumented parents. Acceptable identification materials are required for the

14
parents to get a copy of their U.S. citizen child’s birth certificate. Advocates filed a federal lawsuit, arguing that the
restricted list of acceptable IDs made access to birth certificates impossible for many parents, and thus created
barriers to accessing school and church services for children, and made travel for the children impossible. In July
2016, the parties reached a settlement: the state of Texas agreed that its registrars would accept a number of
types of Mexican identification, including the electoral card, with similar guidelines to be adopted for Central
American countries. The parent must provide two such identification cards, or one such identification card
together with a two supporting documents. While official guidance on the settlement is not yet published, a
much-expanded list of “support docs” will be accepted (to supplement the identification document from the
country of origin), such as insurance cards, bank statements, loan documents, bills, rent receipts, medical records,
church records, and school records.
Readers are encouraged to report any continued problems with birth certificate access, so the court can ensure
that the new policies are being followed.
The Health Insurance Marketplace:
Coverage and Challenges for Immigrant and Mixed-Status Families
Since the Health Insurance Marketplace opened in October of 2013, Texas families that are made up of non-US
citizens, or of individuals with differing citizenship and immigration statuses—“mixed immigration status
families”— have faced all the same barriers to enrollment experienced by native-born uninsured. These included
federal Marketplace web and information technology systems that did not function in October and November
2013, lack of awareness of the available subsidies, confusion over timelines, and more. But immigrant and
“mixed-status” families faced additional potential barriers as well. In a recent nationwide survey of individuals
who assist consumers in the enrollment process, the majority of respondents said that enrollment of immigrants
took twice as long as enrollment of US-born citizens.
ii
Some of the areas of greatest concern and unmet needs
include:
System and Technical Barriers for Immigrant and Mixed-Status Families: Improved But Hurdles Still Exist
During its first few months of operation, the federally facilitated health insurance Marketplace (operated under
the U.S. Department of Health and Human Services (HHS)) used in Texas was initially unable to accurately record
information on immigration documents or to fully process an application for coverage and subsidies for those
households. For some applicants, this resulted in long delays in eligibility decisions, months without coverage, and
no ability for applicants or their advocates to find out about the status of their application, or to get help finalizing
a decision. Since these initial system failures, HHS has made large improvements to the website, and enrollment
into Marketplace coverage has improved. However, many barriers still remain for immigrants and mixed-status
families including:
greater difficulty verifying identity and proving income (e.g., for families headed by recent or
undocumented immigrants),
difficulty entering information related to their immigration status or citizenship documents for those born
outside the U.S., and
applicants with income under the poverty line being incorrectly assessed as potentially eligible for
Medicaid or falling into the Coverage Gap, instead of being determined eligible for subsidies.

15
Verifying Identity and Immigration Status
In a mixed-status family seeking benefits for the U.S. citizen and lawfully present members, but that includes one
or more undocumented earners, verifying whether family members meet income guidelines for Marketplace
benefits can be more challenging. Because the IRS does not rely on historical tax records that are tied to Individual
Taxpayer Identification Numbers (used by some workers without Social Security Numbers to file and pay federal
income taxes) to verify income, some families are required to provide additional income documentation to
complete their applications. In addition, the federal Marketplace’s identity-verification process relies on the use of
credit histories. This is problematic for recent immigrants, young people, and unbanked or underbanked persons,
as they are less likely to have a credit history and therefore must use the longer, manual process to verify their
identity.
For applicants who are lawfully present or who are naturalized citizens, verifying their citizenship or immigration
status can also be difficult, and may take weeks or months to complete. During the first open enrollment, the
Healthcare.gov website systems for real-time immigration verification functioned poorly, requiring families to
mail paper documents to the Marketplace instead. During the second and third open enrollment periods the
website functionality was greatly improved, glitches became less frequent, and HHS created a process for paper
documentation to be uploaded. However, the process for verifying immigration status in real-time still often does
not work even if all information is filled in correctly, and applicants are often required to submit additional
documents to finalize enrollment.
When immigration/citizenship status or income cannot be verified in real-time, most applicants are allowed to
enroll in coverage, but must provide the required documentation within 90 days. This is often called an
“inconsistency period.” If an applicant has an inconsistency related to immigration or citizenship status and she
does not provide the required documentation within the time frame her coverage will be cancelled. For income
inconsistencies, if the required proof of income is not provided the applicant’s subsidies may be cancelled or
reduced, but they will remain enrolled in coverage. Most people in this situation eventually cancel their coverage,
because without subsidies the coverage is unaffordable.
Marketplace Coverage Terminations
After the first open enrollment period due to the many system errors, the federal Marketplace provided
additional time for applicants to finalize the verification of their information. In May 2014, federal Marketplace
officials tried to contact close to a million people nationwide with discrepancies in their immigration and
citizenship records. The great majority submitted (or re-submitted) documents as requested, but about 115,000
of the original number (almost 20,000 in Texas) did not respond by September 2014 to a second outreach
attempt, and lost their coverage the next month. About 4,500 of these consumers had their coverage reinstated
retroactively after they provided the Marketplace with the documents requested.
After the second open enrollment, the Marketplace implemented the tighter time frame policy of providing just
90 days for applicants to clear data inconsistencies for income, immigration status, or citizenship before denying
coverage or adjusting subsidies. In total during 2015, coverage was terminated for about 500,000 consumers
nationwide with citizenship or immigration data matching issues and subsidies. In 2016 the numbers terminated
dropped substantially, to about 17,000 consumers with unresolved citizenship or immigration status data
matching issues. Compared to the first quarter of last year, this represents an 85 percent decrease in the number
of consumers whose coverage ended because of an unresolved citizenship or immigration data matching issue.
If consumers have the appropriate documents but their enrollment through the Marketplace was terminated
based on a citizenship/immigration status data matching issue, they are able to submit their documentation and

16
regain enrollment through the Marketplace outside of the usual open enrollment dates, through a Special
Enrollment Period (read more below).
Communications Barriers
Advocates and enrollment assisters continue to report that the process for providing required documentation
needs improvement. Many consumers reported submitting the same documents multiple times to no effect and
that notices do not clearly explain what information is needed. Furthermore, notices and call center assistance are
only available in English and Spanish and the Marketplace call center translation services for languages other than
Spanish can be cumbersome.
Misdirection
The design of the Marketplace application has caused many adult immigrants who are not eligible for Medicaid in
Texas to be routed unnecessarily to the state Medicaid agency. This additional unnecessary step can significantly
delay Marketplace enrollment. If an immigrant applicant with income below the poverty line indicates on the
application that they are “lawfully present” but the Marketplace is not able to electronically verify that person’s
immigration status (a frequent event), the system may then incorrectly assume that the applicant is either
Medicaid eligible (if they have kids and very low income) or that they are in the Coverage Gap. It will not recognize
that their immigration status makes them ineligible for Texas Medicaid. (Remember, most lawfully present
immigrants in Texas are eligible for Marketplace subsidies even if their income is below the poverty line, because
federal law specifically allows subsidies for legal immigrants below the poverty line, if they are excluded from
Medicaid on the basis of their immigration status.)
The system then assumes their application should be sent to the Texas Health and Human Service Commission for
a Medicaid determination. In a recent nationwide survey, enrollment assisters identified these unnecessary
transfers to state Medicaid agencies of individuals who are not eligible for Medicaid as their top priority for
improvements to the Marketplace application and enrollment process.
iii
“Special Enrollment Periods” and Exceptions to Tax Penalty
As discussed, getting the Marketplace to approve premium subsidies and cost-sharing reductions for lawfully
present immigrants with incomes below the poverty line can be difficult and may take weeks or months. To help
address this issue, HHS made households facing these barriers eligible for a “special enrollment period” (SEP) that
allows them to continue to work with the federal Marketplace until they can get their applications correctly
processed, outside of the annual Open Enrollment period.
In addition to SEPs that help immigrants enroll in coverage, several exceptions to the tax penalty for being
uninsured also protect mixed-status families. Exemptions include special treatment of domestic violence
survivors, families with income low enough that they aren’t required to file taxes, and families who encountered
any one of a wide variety of hardships through the year. Neither the SEPs nor the tax penalty exemptions provide
retroactive coverage for Marketplace insurance, so families who face delays in coverage may still have to deal
with medical debts they accumulated while waiting to get coverage.
Marketplace Affordability in Question for Some Non-Citizens
Lawfully present immigrants in below-poverty income households can (unlike their U.S. citizen neighbors) buy
coverage in the Marketplace. When they do, many can get subsidies that were intended and designed for
households at or above the poverty line. They may pay as much as 2 percent of their income for monthly
premiums, plus additional out-of-pocket amounts when they get services and medications. It is too soon to assess
to what extent these costs may prove prohibitive for families below the poverty line.
17
Policy Barriers that Can Affect any Low-Income Uninsured, Including Immigrants
Several ACA flaws affect both U.S. citizens and lawfully present people. A portion of mixed-status families at
various incomes will also experience the so-called “family glitch.” Federal rules deny subsidies to spouses and
children where one working parent has “affordable” worker-only coverage, even though the out-of-pocket costs
to insure the spouse and children may be prohibitive. This illogical policy is an unintended result of the Internal
Revenue Service’s interpretation of the ACA’s language, and one which can only be fixed if Congress is able to
make corrections to the ACA. The likelihood of Congress achieving technical corrective changes to the ACA has so
far been diminished by the broader political battle over the law, with opponents seeking to repeal the law rather
than improve it.
Another affordability barrier can occur when low-income parents are separated but not divorced, because
Marketplace subsidies are not available for households when a married couple files separate income tax returns.
The high cost of divorce, complex immigration concerns, and cultural attitudes toward divorce all can contribute
to families being cut off from Marketplace subsidies—and affordable comprehensive care—in these situations.
Families with highly unpredictable earnings that may change from week to week or month to month may also
find it more difficult to calculate the right premium subsidies, or to verify their current or predict their future
income. Incomes of workers who are paid routinely with cash or without a formal payroll check may not be
verifiable through online wage databases. Households can get assistance with these challenges, but the need to
resort to manual income documentation can result in delays in coverage for the families with the least resources.
Systems for Resolving Complex Cases Lacking
Finally, the Health Insurance Marketplace website and systems were designed to streamline eligibility and
enrollment for most applicants. However, these systems often do not meet the needs of families with more
complex or non-traditional circumstances such as mixed immigration statuses, non-traditional family structure,
and unpredictable earnings. Currently, the federal Marketplace does not provide a robust support system through
which complex cases can be referred to expert staff and addressed quickly. More should be done to increase the
numbers of trained Marketplace staff that can perform complex casework, and thereby reduce the need to use
the formal appeals process.
Understanding How Families Can Get Caught in the “Family Glitch”
No-Glitch Example:
The Garcia family needs health care for the two parents, Don and Ann, ages 35 and 33, living in Travis County,
TX. Don and Ann are both lawfully present immigrants, and their two school-age daughters are U.S. citizens.
With a family of four and income of $35,600, their income is about 150 percent of the FPL. Their two children
are enrolled in CHIP (with no monthly fee), but neither Don nor Ann’s job offers health benefits.
In the marketplace, Don and Ann qualify for a $352 per month tax credit, allowing them to pay $121 each
month for a health plan that would have cost $473 per month without a subsidy.
Family Glitch Example:
Don’s employer offers a health plan, and pays half of his premium. The employer “offers” coverage for Ann
and the children, but does not pay any of the premium. Under law, because Don’s one-half share of his
worker-only premium is less than 9.5 percent of his family income, Ann and the girls cannot get premium
subsidies in the Marketplace. Fortunately, the girls can get CHIP, but Don and Ann face spending $355 a
month for coverage (half of his job-based premium, plus 100 percent of the cost of her Marketplace plan).
This is 12 percent of their monthly income.
18
Recap: Many Gaps Persist in Access to Care for Immigrants in Texas
With over 4.6 million uninsured Texans in 2015, substantial gaps in access to health care will remain a problem for
many Texans in the near term, despite the important gains and new options provided by the ACA. Listed below is
a partial inventory of notable holes in the Texas health care safety net for non-U.S. citizen residents.
Undocumented
The greatest access gaps for non-citizens affect Texans without legal immigration status. Barred from Medicaid,
CHIP, and the Marketplace and its subsidies, private health coverage is available only to undocumented
individuals who have adequate income to purchase a policy at full price, without a subsidy. Undocumented
residents can look to Federally Qualified Health Centers, some (but not all) urban hospital/health districts, and
independent charity clinics for care, meaning that access to affordable care is highly variable depending on
where an immigrant lives in Texas.
Lawfully present
Immigrants who are lawfully present in the U.S. face certain barriers that are specific to their non-citizen status, as
well as some of the same barriers affecting U.S. citizens.
The Coverage Gap traps some lawfully present, including refugees and asylum seekers. Most lawfully
present individuals with incomes below 100 percent of the FPL can qualify for subsidies in the ACA
Marketplace. However, certain lawfully present immigrants are caught in the Coverage Gap in states like
Texas that have not accepted federal ACA funds to extend Medicaid to adults who earn less than 138
percent of the FPL. So the categories of legal immigrants that Congress intended in 1996 to have access
to Medicaid and CHIP, actually are the very ones who are left without coverage options in Texas and
other states that have not expanded Medicaid.
Texas law excludes most lawfully present immigrant adults from Medicaid. The state legislature would
have to authorize a change to this state policy (adopted in 1999) in order for a Texas solution to insure
low-income Texans in the Coverage Gap to also benefit lawfully present adults below the poverty line.
Technical Marketplace application processing issues for individuals with immigration documents, as well
as for mixed-status families have delayed coverage and discouraged eligible Texans from completing
enrollment. Improved Marketplace performance during the second and third open enrollment period
appears to be improving enrollment rates but further improvement is still needed.
The “family glitch” affects both lawfully present immigrants and U.S. citizens. These families may not
qualify for premium subsidies in the Marketplace , and face either paying full price and an unlimited,
unaffordable percentage of their incomes for job-based or Marketplace insurance premiums, or
remaining uninsured.
Affordability issues occur even for families that have access to premium subsidies and out-of-pocket help
in the Marketplace. Those below poverty may have a hard time affording 2 percent of income in
premiums with additional copayments and deductibles. Families at any income level who experience high
health care needs may face spending up to 20 percent of income before deductibles and out-of-pocket
caps kick in.
Separated, but not divorced, parents may not have access to Marketplace subsidies because of tax filing
status or lack of access to income information on the absent spouse.
19
Hard-to-verify incomes. The income verification systems that the Marketplace and state Medicaid-CHIP
programs rely on can work well for those with steady employment and predictable hours and wages. They
are less helpful for those working irregular hours, multiple jobs, or being paid cash or by hand-written
check. Advocates will need to monitor the systems to identify and try to reduce any barriers to
enrollment, renewal, or qualifying for premium subsidies that may result from the additional
documentation families in these situations may have to produce on an ongoing basis.
As we publish this report in late 2016, few solutions to the barriers listed above are truly in the pipeline. In the
Marketplace open enrollment periods for 2015 and 2016 coverage, systems to accept immigration documents
from lawfully present family members were working substantially better than in the first period. Still, large
numbers of families face multiple barriers in the Marketplace. Application assisters report families who struggled
to complete applications in a previous year lack confidence that their information will be processed promptly and
accurately in the next year.
Apart from gradual technological improvements, the remaining barriers will require concerted attention and
advocacy at the state and federal levels, as well as local solutions to maintain or expand safety nets for the
undocumented residents who are excluded from state and federal programs.
Protecting Access in Your Texas Community:
How You Can Help, and How to Get Help
As noted at the opening of this report, a number of policy challenges to immigrants’ access to care have
arisen in Texas over the last two years. Legislation to reduce access to care for undocumented children in
Texas’ Children with Special Health Care Needs Program was filed and only narrowly defeated in 2015. The
Department of State Health Services was served with a lawsuit, after some local officials stopped issuing
birth certificates to undocumented parents of U.S. citizen children (positive settlement reached July 2016).
Tom Green County requested a state Attorney General’s opinion on whether counties should discontinue
services to undocumented residents in the County Indigent Health Care Program. In related matters,
interim legislative studies were charged with examining state and local laws applicable to undocumented
immigrants, and questioning Texas’ official involvement in the Refugee Resettlement Program. In
September 2016, Texas Governor Greg Abbott announced that Texas will withdraw from the federal
refugee resettlement program.
iv
A new presidential administration will take office in January 2017, which based on its campaign rhetoric
may be expected to promote harsher public policy toward non-U.S. citizens, and could weaken the
existing federal protections of the rights of immigrants.
In light of these recent pressures, CPPP hopes this report will help community organizations, health care
providers, and other stakeholders interested in supporting access to health care for all members of the
community. The Center can also offer support in two other ways:
Group training on the policies in this report, in your community or via webinar; and
Trouble-shooting assistance when you have questions about whether laws and rules are being
followed regarding immigrants’ access to coverage or care.
To inquire about training or other assistance for your organization, please contact CPPP at
dunkelberg@cppp.org.

20
Next Steps for Texas: Policies to Improve Health Care Access and Outcomes
Federal law, Texas law and the state constitution combine to make Texas cities, counties, and hospitals the
providers and funders of last resort for all of the uninsured. U.S. and Texas law allow federal and state
government to reject the health costs of uninsured immigrants—lawfully present and undocumented alike—and
shift them to local governments and health care providers. In this way, Texas’ policy decisions to turn down
available federal support for the uninsured take a toll on local taxpayers, and on all the other services
communities need to fund.
CPPP recommends that Texas make the following three key policy changes to increase federal funding for
coverage and care of immigrants:
1. Providing Medicaid Maternity benefits to lawfully present immigrant women. Texas should provide
comprehensive pregnancy benefits on par with those of U.S. citizens. Today, even legal permanent residents
are treated the same as undocumented mothers.
2. Closing the Texas Coverage Gap, and insuring all citizens 19-64 up to 138 percent of the federal poverty line
($27,724 for a family of 3). This step would do even more than #1 for maternal health, by allowing women
access to medical homes before conception for healthier pregnancies, continuing their care after birth to
screen for and treat chronic medical conditions, and thereby improving health for any future pregnancies.
This improved care will be gained equally if accomplished via an 1115 “red state waiver” conservative
alternative.
Closing the Gap will also eliminate today’s perverse policy which denies access to coverage to immigrants
Congress intended to protect: e.g., active-duty military and veterans, victims of human trafficking, and
refugees. Step #2 will also dramatically improve payments to hospitals and doctors for emergency care to
uninsured undocumented residents.
3. Providing Medicaid benefits to lawfully present immigrants aged 19 and older. Lawmakers should also
reverse the Texas law that now excludes these adults, in order to maximize the reduction in uninsured
lawfully present Texans and the relief for local governments that closing the Coverage Gap would bring. Texas
Medicaid today covers very few U.S. citizen parents and adults under current policy: e.g., 3 million children
are enrolled, but only 150,000 of their parents. Unless Texas begins providing coverage options for U.S. citizen
parents and other adults living in poverty, reversing Texas’ ban on Medicaid for lawfully present immigrant
adults will have limited effect.
Of course, the steps described above do not fully address the barriers to care for undocumented residents and the
costs of their care born by local governments and care providers. Texas should take the lead among the states,
squarely face the realities and negative consequences of these barriers for our communities, and develop a
proactive strategy to improve systems and financing of care for the undocumented uninsured.
21
Helpful Resources
Center on Budget and Policy Priorities, Health Reform Beyond the Basics; slide decks provide detailed
information on application and eligibility issues and processes;
http://www.healthreformbeyondthebasics.org/category/issues/immigrant-eligibility-for-premium-tax-credits-
and-medicaid/
A Comprehensive Review of Immigrant Access to Health And Human Services
http://aspe.hhs.gov/hsp/11/immigrantaccess/review/index.pdf
Overview of Immigrant Eligibility for Federal Programs – see page 4 for a list of “qualified” immigrants.
http://www.nilc.org/document.html?id=108
Getting Enrollment Right for Immigrant Families; http://ccf.georgetown.edu/ccf-resources/getting-enrollment-
right-immigrant-families/
Immigrants and the ACA - http://nilc.org/immigrantshcr.html; http://nilc.org/immigrantshcrsp.html ;
https://www.healthcare.gov/what-do-immigrant-families-need-to-know/
Sponsored Immigrants & Benefits - http://www.nilc.org/document.html?id=166
“Lawfully Present” Individuals Eligible under the Affordable Care Act -
http://www.nilc.org/document.html?id=809
Frequently Asked Questions – Exclusion of Youth Granted “Deferred Action for Childhood Arrivals” from
Affordable Health Care - http://www.nilc.org/document.html?id=802
Verification & documentation - http://nilc.org/document.html?id=35 ;
https://www.healthcare.gov/help/immigration-document-types/ ; https://www.healthcare.gov/help/citizenship-
and-immigration-status-questions/
Federal Guidance on Public Charge – When Is it Safe to Use Public Benefits? -
http://www.nilc.org/document.html?id=164
Confidentiality and reporting fears - http://www.ice.gov/doclib/ero-outreach/pdf/ice-aca-memo.pdf
Linguistic and cultural barriers - https://www.cuidadodesalud.gov/es/ ;
http://marketplace.cms.gov/getofficialresources/other-languages/other-languages-materials.html ;
http://www.hhs.gov/open/execorders/13166/index.html
22
Appendix: Deeper Background on Federal Policy on Immigrants’ Access to Health Care
Federal immigration and welfare laws passed in 1996 and after have made big changes to non-US citizens’ access
to health care and safety net services, for both lawfully present immigrants and for those lacking legal status. The
complex intersection of health care and immigration laws makes it challenging for health consumers and
professionals to master the landscape of access to care for non-US citizens. The 1996 law and changes added by
the Affordable Care Act have resulted in a very complex web of eligibility rules and exclusions, and readers who
seek full details are strongly encouraged to consult the source materials cited and at the end of this brief.
Welfare Law Brings Health Care Limits
In 1996, Congress passed a welfare law, the Personal Responsibility and Work Opportunity Reform Act (PRWORA),
that affected legal immigrants’ eligibility for health and human services.
Before the 1996 law, most legally present immigrants had been treated essentially the same as U.S. citizens for
these programs, but after the law took effect the rules became much more complex.
The law coined new terms such as “qualified” and “not qualified” immigrants, to categorize immigrants according
to eligibility for health and human services benefits.
1. a number of legal immigration statuses were designated for the first time as “not qualified” for
benefits, and essentially treated the same as undocumented immigrants for purposes of benefit
eligibility even though they were lawfully present in the U.S.;
2. despite what the name suggests, many “qualified immigrants” were excluded from eligibility in
significant ways; and
3. big differences in eligibility depended on whether an immigrant had entered the U.S. prior to the
8/22/96 date when PRWORA was signed.
“Qualified/Not Qualified” Legal Immigrants, PRWORA 1996
Qualified
Not Qualified
(1) Lawful permanent residents (LPRs);
(2) Refugees, those granted U.S. asylum, those granted withholding of
deportation/removal, conditional entry (in effect prior to Apr. 1, 1980), or paroled into
the U.S. for at least one year;
(3) Cuban/Haitian entrants;
(4) Battered spouses and children with a pending or approved (a) self-petition for an
immigrant visa, or (b) immigrant visa filed for a spouse or child by a U.S. citizen or LPR,
or (c) application for cancellation of removal/suspension of deportation, whose need
for benefits has a substantial connection to the battery or cruelty (parent/child of such
battered child/spouse are also “Qualified”); and
(5) Victims of trafficking and their derivative beneficiaries (for example, children of
victims) who have obtained a T visa or whose application for a T visa “sets forth a prima
facie case,” meaning they make certain claims and meet specific preliminary
documentation. (NOTE: A broader group of trafficking victims who are certified by or
receive an eligibility letter from the Office of Refugee Resettlement are eligible for
benefits funded or administered by federal agencies, without regard to their
immigration status.)
Includes all noncitizens who do not
fall under the “Qualified”
immigrant categories.
This includes undocumented
persons, but also (for example)
these lawfully present groups:
Employment Visas (including
agricultural); Temporary Protected
Status; Lawful Temporary
Residents; Family Unity Status;;
Non-immigrants (tourists,
students, survivors of serious
crimes), individuals granted
deferred action; with pending
applications for asylum; applicants
for adjustment to lawful
permanent residence.
Source: National Immigration Law Center, Overview of Immigrant Eligibility for Federal Programs–see page 4 for a list of
“Qualified” immigrants.

23
Some qualified immigrants have fewer restrictions than others
There are several situations in which people with a “qualified immigrant” status are treated just like a U.S. citizen
when it comes to getting Medicaid. These exceptions include:
Active-duty U.S. military and veterans (and their spouse and dependent children);
Humanitarian statuses: refugees, those granted U.S. asylum, withholding of deportation, Cuban & Haitian
entrants, are not excluded from Medicaid during their first 7 years in U.S.; and
Lawful permanent residents with credit for 10 years (40 quarters) of U.S. work history.
Undocumented Then, Lawfully Present Now
Immigrants who came to U.S. before 8/22/96 without legal status, but later became a qualified immigrant can be
treated as a pre-1996 immigrant if they have resided in the U.S. continuously. In this situation, an immigrant is
considered to have “continuously” resided if they never left the U.S. for more than 30 days at one time, or for
more than 90 days total, between August 22, 1996, and when they became a qualified immigrant. This is
important because pre-1996 immigrants in Texas are eligible for many benefits that post-1996 entrants cannot
get. It is a situation that may affect survivors of domestic abuse as well as human trafficking.
PRWORA Limits Medicaid Eligibility
The 1996 law classified (regular, non-emergency) Medicaid as a “federal means-tested public benefit,” and
declared that most newly-arrived qualified immigrants would be subject to a “five-year bar” before they could
access Medicaid. Importantly for Texas, federal law and rules gave states these choices:
1. whether to allow Medicaid access for qualified immigrants after they have been in the U.S. for five years;
and
2. the option to make different choices on #1 above for pre- and post-PRWORA immigrants.
PRWORA Effect on other Federally Funded Public Health Programs
Other health-related federal funding programs were classified differently under the 1996 law from Medicaid-
CHIP, and federal guidance made clear that there were no restrictions on lawfully present immigrants' access to
other federal programs such as those dedicated to maternal and child health, mental health, family planning, and
immunization. Federal guidance also prohibited restricting access to these key public health programs for most
undocumented residents.
Balanced Budget Act requires coverage in “stand-alone” CHIP
When Congress established CHIP in the Balanced Budget Act of 1997, states had choices: first, whether to set up
a CHIP program at all, and second whether to set up CHIP as a separate program from children’s Medicaid (as
Texas did), or to simply make CHIP an extension of children’s Medicaid. Importantly, states with separate CHIP
programs were required to allow qualified immigrant children and teens (under age 19) to enroll in CHIP after
they have passed their five-year bar.
2009: CHIPRA provides state option to cover “Lawfully Present” children and pregnant women; ACA
adopted same “lawfully present” definition for Marketplace. In 2009, the Children’s Health Insurance
Program Reauthorization Act (CHIPRA) was signed into federal law. CHIPRA expanded the categories of
immigrants who may gain access to Medicaid and CHIP, at state option: “lawfully present” residents of a state.
CHIPRA gave states the option to cover children and pregnant women in Medicaid and CHIP without the five-year

24
bar imposed in 1996. (CHIPRA also exempted children and pregnant women in Medicaid and CHIP from the
deeming of sponsor income, and from sponsor liability for the costs of their coverage.)
Soon afterward, the ACA was signed into law, and used the same lawfully present grouping to define the
immigrants eligible for participation and affordability help in the health insurance Marketplaces that were
launched in 2014.
The lawfully present grouping is, as the name suggests, broader than the 1996 qualified immigrant grouping.
Virtually all immigrants with a legal status are included in the CHIPRA state options for lawfully present pregnant
women and children, assuming they can also meet other program requirements like income and residency.
DACA “DREAMers” Excluded
The notable exception to the “lawfully present” grouping is the exclusion of immigrant youth “granted relief”
under the Deferred Action for Childhood Arrivals (DACA). DACA grants relief from deportation and potentially
allows short-term work authorization to undocumented youth and young adults who entered the U.S. before age
16 and who meet other criteria. For immigration and virtually any other purpose, DACA grantees are lawfully
present in the U.S. However, they were excluded from the lawfully present definition used in determining
eligibility for Medicaid, CHIP (under the CHIPRA option), and the Marketplace affordability programs. Individuals
granted deferred action based on any other grounds (other than DACA) are included in the health care programs’
definition of lawfully present.
For complete listings of lawfully present immigration statuses, see “Lawfully Present” Individuals Eligible under
the Affordable Care Act; and Healthcare.gov https://www.healthcare.gov/help/immigration-status-questions/.
ACA’s Basic Health Plan Option
The ACA includes an option, available only to states that have implemented adult Medicaid Expansion or a related
waiver, called the Basic Health Plan (BHP). Like a CHIP program for adults, BHP can cover state residents under
age 65 with incomes over 133 percent but not exceeding 200 percent of the federal poverty level. The BHP option
can also cover lawfully present immigrants who are not eligible for Medicaid with incomes between zero and 200
percent of the FPL.
i
45 CFR §155.315 (d)(4) Verification process related to eligibility for enrollment in a QHP through the Exchange; 42 CFR
§435.956 (c)(2) Verification of other non-financial information.
ii
S. Schwartz & T. Brooks, “Getting Enrollment Right for Immigrant Families,” Georgetown University Center for Children and
Families (February 2016).
iii
Ibid.
iv
“If Texas withdraws from the federal refugee resettlement program, it doesn't mean refugees would stop flowing to the
state; the federal government could distribute money directly to nonprofit groups here. Resettlement officials have said the
U.S. Refugee Act of 1980 allows the federal government to designate an entity other than a state government to serve as the
state refugee coordinator and disburse funding — a set-up currently in place in six states.” Texas Tribune, September 21,
2016.
